Rotator Cuff Tear
Shoulder injuries are pretty common. Each year, approximately 200,000 Americans require shoulder surgery to repair a torn rotator cuff and an additional 400,000 have surgery for related tendonitis or partial tears. Dr. Fyda, a Board Certified Orthopaedist who is fellowship trained in Sports Medicine, completes about 150 rotator cuff surgeries a year in Reno. Most of the injuries he and other orthopaedists see are related to the wear and tear of age. However, those that rely heavily on their shoulders – athletes who throw and those who do heavy manual labor – are more prone to injury. Some studies have found the prevalence of rotator cuff tears may exceed 50 percent in people over 65.
What is the rotator cuff?
Your arm is kept in your shoulder socket by your rotator cuff. The rotator cuff is a network of four muscles that come together as tendons to form a covering around the head of the humerus, or upper arm bone. The rotator cuff attaches the humerus to the shoulder blade and helps to lift and rotate your arm.
There is a lubricating sac called a bursa between the rotator cuff and the bone on top of your shoulder (acromion). The bursa allows the rotator cuff tendons to glide freely when you move your arm. When the rotator cuff tendons are injured or damaged, this bursa can also become inflamed and painful.
Injury description
When one or more of the rotator cuff tendons is torn, the tendon no longer fully attaches to the head of the humerus. A torn rotator cuff will weaken your shoulder making typical activities, like combing your hair or getting dressed, painful and difficult.
In many cases, torn tendons begin by fraying. As the damage progresses, the tendon can completely tear, sometimes with lifting a heavy object.
There are different types of tears.
- Partial Tear - This type of tear damages the soft tissue, but does not completely sever it.
- Full-Thickness Tear - This type of tear is also called a complete tear. It splits the soft tissue into two pieces. Often the tendon tears off where it attaches to the head of the humerus leaving a hole in the tendon.
Injury causes
There are two main causes of rotator cuff tears: injury and degeneration.
Acute Tear
If you fall down on your outstretched arm or lift something too heavy with a jerking motion, you can tear your rotator cuff. This type of tear can occur with other shoulder injuries, such as a broken collarbone or dislocated shoulder.
Degenerative Tear
Most tears result from a wearing down of the tendon that occurs slowly as we age. Rotator cuff tears are more common in the dominant arm. If you have a degenerative tear in one shoulder, there is a greater risk for a rotator cuff tear in the opposite shoulder – even if you have no pain in that shoulder.
Several factors contribute to degenerative, or chronic, rotator cuff tears.
- Repetitive stress - Baseball, tennis, rowing, and weightlifting are examples of sports activities that can stress your rotator cuff muscles and tendons and put you at risk for overuse tears.
- Lack of blood supply - As we get older, the blood supply in our rotator cuff tendons lessens. Without a good blood supply, the body's natural ability to repair tendon damage is impaired.
- Bone spurs - As we age, bone spurs (bone overgrowth) often develop on the underside of the acromion bone. When we lift our arms, the spurs rub on the rotator cuff tendon. This condition is called shoulder impingement, and over time will weaken the tendon and make it more likely to tear.
Risk Factors
- Age
- People who do repetitive lifting or overhead activities – e.g. painters, carpenters,
- Athletes, particularly tennis players and baseball pitchers
- Traumatic injury
Symptoms
- Pain at rest and at night, particularly if lying on the affected shoulder
- Pain when lifting and lowering your arm or with specific movements
- Weakness when lifting or rotating your arm
- Crackling sensation when moving your shoulder in certain positions
- Tears that happen suddenly, such as from a fall, usually cause intense pain. There may be a snapping sensation and immediate weakness in your upper arm.
Diagnosing
Your doctor will test your range of motion by having you move your arm in different directions. He or she will also check to see whether it is tender in any area or whether there is a deformity.
Imaging Tests
Other tests a doctor may use to confirm a rotator cuff diagnosis:
- X-rays - The first imaging tests performed are usually x-rays. Because x-rays do not show the soft tissues of your shoulder like the rotator cuff, plain x-rays of a shoulder with rotator cuff pain are usually normal or may show a small bone spur.
- Magnetic Resonance Imaging (MRI) or Ultrasound - These studies better show soft tissues like the rotator cuff tendons. They can show the rotator cuff tear, as well as where the tear is located within the tendon and the size of the tear.
Treatment
If you have or suspect you have a rotator cuff tear, see a qualified orthopaedist. If you keep using a damaged shoulder, you may cause further damage and exacerbate the tear.
There is no evidence of better results from surgery performed near the time of injury versus later on. For this reason, many doctors first recommend nonsurgical management of rotator cuff tears.
Nonsurgical Treatment
In about 50% of patients, nonsurgical treatment relieves pain and improves function in the shoulder. Shoulder strength, however, does not usually improve without surgery. Nonsurgical treatment options may include:
- Rest. Your doctor may suggest rest, limiting overhead activities and wearing a sling.
- Activity modification. Avoid activities that cause shoulder pain.
- Non-steroidal anti-inflammatory medication. Drugs like ibuprofen and naproxen reduce pain and swelling.
- Strengthening exercises and physical therapy. Specific exercises will restore movement and strengthen your shoulder. Your exercise program will include stretches to improve flexibility and range of motion.
- Steroid injection. If rest, medications, and physical therapy do not relieve your pain, an injection of a local anesthetic and a cortisone preparation may be helpful. Cortisone is a very effective anti-inflammatory medicine.
A nonsurgical treatment will not improve strength and the tear may increase over time further limiting activities.
Surgical Treatment
The decision to perform surgery varies from physician to physician. Some will assess pain and function levels over the course of six months. Dr. Fyda of Great Basin Orthopaedics will typically recommend surgery when a symptomatic complete tear fails to respond to non-surgical treatment. He believes that delaying surgery excessively may compromise the final outcome.
Surgery to repair a torn rotator cuff most often involves re-attaching the tendon to the head of humerus (upper arm bone). A partial tear, however, may need only a trimming or smoothing procedure called a debridement. A complete tear within the thickest part of the tendon is repaired by stitching the two sides back together.
Many surgical repairs can be done on an outpatient basis and do not require you to stay overnight in the hospital. Your orthopaedic surgeon will discuss with you the best procedure to meet your individual health needs.
There are three commonly used techniques for rotator cuff repair and all are well rated by patients for pain relief, strength improvement, and overall satisfaction.
Open Repair
A traditional open surgical incision (several centimeters long) is often required if the tear is large or complex. The surgeon makes the incision over the shoulder and detaches the shoulder muscle (deltoid) to better see and gain access to the torn tendon.
All-Arthroscopic Repair
During arthroscopy, your surgeon inserts a small camera, called an arthroscope, into your shoulder joint. Because the arthroscope and surgical instruments are thin, your surgeon can use very small incisions and this is considered a minimally-invasive procedure performed as an outpatient procedure. The majority of Dr. Fyda’s rotator cuff surgeries are outpatient arthroscopic procedures and his experience indicates patient comfort is substantially better compared to open or mini-open repairs.
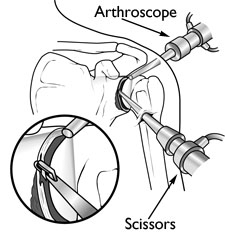
During arthroscopy, your surgeon inserts the arthroscope and small instruments into your shoulder joint.
Mini-Open Repair
The mini-open repair uses newer technology and instruments to perform a repair through a small incision. The incision is typically 3 to 5 cm long. This technique uses arthroscopy to assess and treat damage. Bone spurs, for example, are often removed arthroscopically. This avoids the need to detach the deltoid muscle.
Once the arthroscopic portion of the procedure is completed, the surgeon repairs the rotator cuff through the mini-open incision. During the tendon repair, the surgeon views the shoulder structures directly, rather than through the video monitor.
Rehabilitation
Physical therapy is essential to help regain shoulder strength and motion.
- Immobilization
After surgery, therapy progresses in stages. At first, the repair needs to be protected while the tendon heals. To keep your arm from moving, you will most likely use a sling and avoid using your arm for the first 4 to 6 weeks.
- Passive Exercise
Even though your tear has been repaired, the muscles around your arm remain weak. Once your surgeon decides it is safe for you to move your arm and shoulder, a therapist will help you with passive exercises, supporting your arm during movement, to improve range of motion in your shoulder. In most cases, passive exercise is begun within the first 4 to 6 weeks after surgery.
- Active Exercise
After 4 to 6 weeks, you will progress to doing active exercises without the help of your therapist. At 8 to 12 weeks, your therapist will start you on a strengthening exercise program.
Expect a complete recovery to take several months. Most patients have a functional range of motion and adequate strength by 4 to 6 months after surgery. Although it is a slow process, your commitment to rehabilitation is key to a successful outcome.
Outcome
The majority of patients report improved shoulder strength and less pain after surgery for a torn rotator cuff. Each surgical repair technique (open, mini-open, and arthroscopic) has similar results in terms of pain relief, improvement in strength and function, and patient satisfaction.
After rotator cuff surgery, a small percentage of patients experience complications. In addition to the risks of surgery in general, such as blood loss or problems related to anesthesia, complications of rotator cuff surgery may include:
- Nerve injury. This typically involves the nerve that activates your shoulder muscle (deltoid).
- Infection. Patients are given antibiotics during the procedure to lessen the risk of infection.
- Deltoid detachment. During an open repair, this shoulder muscle is detached to provide better access to the rotator cuff. It is stitched back into place at the end of the procedure. It is very important to protect this area after surgery and during rehabilitation to allow it to heal.
- Stiffness. Early rehabilitation lessens the likelihood of permanent stiffness or loss of motion.
- Tendon re-tear. There is a chance for re-tear following all types of repairs. The larger the tear, the higher the risk of re-tear. Repeat surgery is needed only if there is severe pain or loss of function.
Sources
American Academy of Orthopedic Surgeons website, http://orthoinfo.aaos.org/topic.cfm?topic=a00064
WebMD website, “Rotator Cuff Tear,” http://www.webmd.com/fitness-exercise/guide/rotator-cuff-tear